Over 250,000 brain tumours are diagnosed across the globe each year. Although aggressive treatment options are available like surgery, radiation and chemotherapy, they can be dependent on the size and location of the tumour, and there is usually only a limited time estimate given to the patient to live.
Inspired by his PhD supervisor who was diagnosed with a brain tumour, Dr. Jeremy Brown was determined to create a better and more precise way to treat these tumours. And that determination led to the creation of a tiny device that could prove to be a game changer in how cancer is treated.
“My PhD supervisor, Dr. Geoff Lockwood, was one of the pioneers of ‘high-resolution ultrasound’ and sort of a world-renowned innovator in ultrasound technology,” says Dr. Brown. “After my PhD, he was diagnosed with a glioblastoma brain tumour and given just one or two years to live following surgery. When he told me that his cancer was terminal, I just couldn’t believe that there was nothing that could be done.
“As a result, I started to look into this particular pathology more and more to see where improvements in treatment and patient survival could be made,” continues Dr. Brown. “Inevitably, it led to a shift in my research focus as I saw there was an unmet need in this area.”
Dr. Brown is an affiliate scientist at Nova Scotia Health in the Department of Surgery, and a professor in Dalhousie University’s School of Biomedical Engineering and Department of Electrical Engineering. What he has created is the world’s first high-resolution endoscopic surgical and imaging probe. Only three millimetres by three millimetres in size, it uses an ultrafast imaging platform, which allows surgeons to use real-time, high-resolution imaging to detect and reach brain tumours.
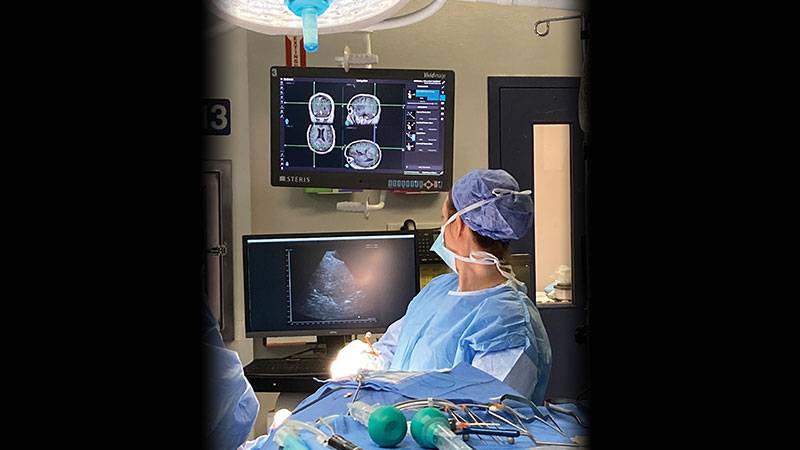
Currently, MRI or CT scans are heavily relied upon to plan an accurate surgical route. While these are incredibly helpful, there are instances where the brain moves inside the cranium after the MRI has been taken, which can make the original image not as precise as needed. Dr. Brown’s device, inserted through a small keyhole created in the skull, is able to provide images that not only allow surgeons to follow an exact path to the tumour, but also help them avoid cutting into healthy tissue and determine if they have left any small pieces of the tumour behind. Eventually these kinds of precise images could allow surgeons to adapt surgical plans on the spot, if needed, and provide them with a reliable way to confirm all cancerous tissue has been removed in the operating room.
The endoscopic and imaging probe was used successfully in the first two in-human surgeries at the QEII Health Sciences Centre earlier this spring. One of the surgeries was a resection of a brain tumour, and the other involved closing off a brain aneurysm.
“It has truly been a pleasure working with Jeremy and his team as they develop this novel ultrasound probe,” says Dr. Adrienne Weeks, a neurosurgeon with Nova Scotia Health and assistant professor in Dalhousie University’s Faculty of Medicine.
But that’s not all this device can do. It will also include a therapeutic tool that will non-invasively vaporize cancerous tissue (essentially turning it into gas bubbles) without the use of heat. This will save healthy tissue from potentially getting damaged and has also been proven to initiate a pretty substantial immune response.
“Essentially when tumours are disrupted, they release tumour antigens (essentially tumour debris) that trigger an immune response that ideally ends up with a variety of tumour-attacking T-cells infiltrating and clearing out the remainder of the tumour cells,” says Dr. Brown. “Histotripsy has been shown to trigger this response much more strongly than other tumour treatment methods. It’s widely thought that this is a result of the combination of non-thermal mechanical disruption of the tumour and the very fine scale of the particles in the debris left over.”
Dr. Brown and his team have already been conducting tests with this new tool in the lab and hope to roll it out soon.
And looking forward, Dr. Brown believes that the ultrasound device could also be beneficial for spinal surgeries. Since these kinds of surgeries require a slightly different angle than brain surgeries, he and his team have already re-designed and successfully fabricated a prototype of the probe.
“I’m working with Dr. Sean Christie, a spine surgeon with a dual appointment at Nova Scotia Health and Dalhousie University, to validate this pre-clinically and then on patients,” says Dr. Brown. “Since it is a very minor modification to the brain probe it should be straightforward to obtain approval for use during spine surgery as well.”
At publication, Dr. Brown and Dr. Christie are awaiting approval from Nova Scotia Health’s Research Ethics Board to use the modified probe for spinal surgeries. Dr. Brown expects up to 15 brain or spine surgeries to be completed with help of the device by the end of 2022.
It’s clear that this tiny device will have a huge impact on how surgeries on the brain and spine are conducted going forward.
“I think it will become an important and valuable tool in the neurosurgery toolbox. It was really exciting to use this for the first time on a patient in the operating room,” says Dr. Weeks.