For half of Canadian cancer patients, treatment comes by way of radiation therapy — beams of energy that are fired through the body to collide with the tumour in question. For the tumour itself, the intended result is death, but for the healthy tissue which surrounds it, radiation exposure is anything but ideal. So for the medical professionals delivering these doses, aim is everything.
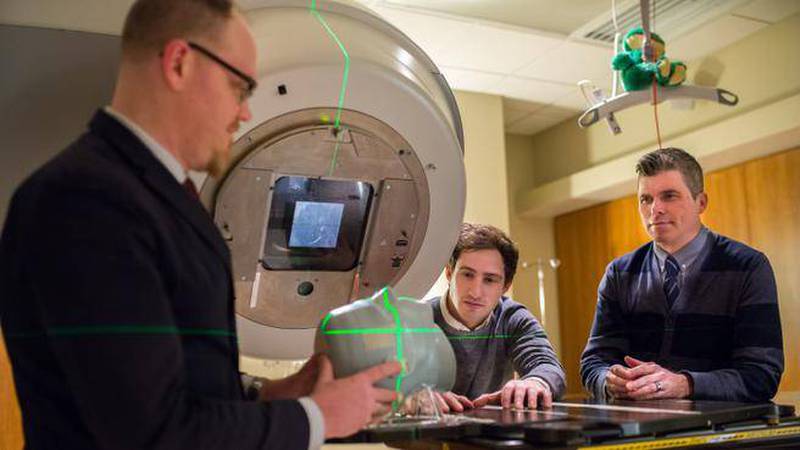
Medical physicists, such as Dr. Chris Thomas, are responsible for the accuracy of these radiation doses, as well as quality assurance for the techniques and technologies involved.
“The best path to a tumour is not always the shortest, because we have what are called organs at risk,” says Dr. Thomas. “You want to avoid irradiating normal healthy tissue as much as possible and different tissues have different tolerances.”
If the beam were to cross the spine, for example, it could result in paralysis, he says. In the optic nerve: blindness; in the lens of the eyes: cataracts; in the lungs: pneumonitis. For this reason, the path, duration and frequency of radiation treatments are critical details, mapped out with great accuracy ahead of time using CT scans and treatment planning software.
Dr. James Robar, chief of medical physics, says the QEII administers 2,700 courses of radiation therapy per year. The service covers the entire province, with assistance from a sister clinic in Sydney.
Helping these medical physicists in their continuing effort to take better aim is a graduate student by the name of Lee MacDonald. He is working toward his PhD in the medical physics graduate program at Dalhousie University led by Dr. Robar himself. This program is one of only 12 in the world to offer masters, doctoral, certificate and residency programs all in one — the whole package.
“We now have the complete educational pathway in Atlantic Canada,” says Dr. Robar.
Beginning in the second year of this partnership’s masters program, students focus their attention on research and in 2013, Lee gravitated toward the cutting edge. Together with Drs. Robar and Thomas, he began work on what is referred to in the field as Four-Pi.
The QEII’s linear accelerators, many funded through the QEII Foundation’s
“We’ve seen reductions in doses to normal tissue of up to 20 per cent,” says Dr. Thomas, quoting from the studies they’ve since carried out using Lee’s algorithms.
To be clear, Dr. Robar says that in none of their studies has this algorithm been used in the treatment of actual patients. While software using aspects of Lee’s algorithms is available commercially, hardware and software manufacturers need to incorporate some technological advances and apply for regulatory approval to implement the full technology that Lee has developed.
Thanks to the efforts of Doris Grant, associate director of Dalhousie’s Industry Liaison and Innovation office, Lee’s refined Four-Pi algorithm was licensed by the medical technology company BrainLab in January 2016. BrainLab has since released an early version of the software which is now available globally, if not necessarily in use just yet.
“Besides lowering the dose to normal tissues, I think one of the most important points of this technology is that it’s increasing the uniformity of the quality of care among practitioners across the world,” says Dr. Robar. “With current techniques, the quality of the treatment plan really depends on the quality of the treatment planner. Some may be new to the job, some may have decades of experience. This algorithm is a systematic and automated way to develop a high quality treatment plan every time.”