The QEII Health Sciences Centre became the first hospital in the Maritimes to use a new prostate biopsy technology last fall — providing urologists with another effective tool to detect prostate cancer, the most common form of cancer in men.
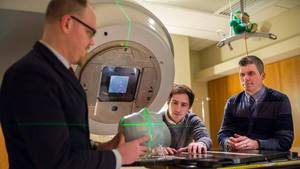
Thanks to a collaboration between the departments of urology and diagnostic imaging, Nova Scotia Health’s Information Management and Technology team and the QEII Foundation, the QEII purchased new magnetic resonance imaging (MRI) fusion technology.
“This is something Nova Scotia needs,” says Dr. Greg Bailly, head of urology for Nova Scotia Health. “This is a perfect example of Nova Scotia Health recognizing and committing to innovation and technology in its investment in improving health care.”
The technology — first used on a patient at the QEII in September 2022 — works by fusing MRI images of the prostate with ultrasound-guided biopsy images. This new technology provides doctors with the precise location of an abnormality that was detected by the MRI, on live ultrasound images during the ultrasound-guided prostate biopsy (removing tissue samples from the prostate for testing).The innovative technology is available to some men from across the Maritimes who have a referral from their urologist.
“In select men who meet specific criteria, MRI can be a highly useful tool in detecting prostate cancer,” says Dr. Andreu Costa, a QEII radiologist who performs biopsies using the modern technology. “MRI allows us to detect cancer with more confidence and accuracy.”
By increasing the accuracy of a biopsy, the MRI fusion technology not only increases the ability to detect cancer earlier and more accurately in some cases, but it often decreases the number of biopsies required, thereby decreasing the risk of infection during a biopsy, says Dr. Costa.
One in seven men in Canada will be diagnosed with prostate cancer in their lifetime. If found early, it can be treated more effectively, with better health outcomes.
Currently, the standard practice to detect prostate cancer is through a prostate-specific antigen (PSA) blood test, a digital rectal exam and ultrasound biopsies. Approximately 500 prostate biopsies are conducted each year in Nova Scotia Health’s Central Zone. Dr. Costa estimates about 100 men will undergo prostate biopsy using the new technology in its first year.
In some cases, prostate cancer is particularly hard for doctors to detect. The MRI fusion technology gives them greater ability to detect cancer in cases where it may not have immediately been found using other techniques. Being able to detect cancer and give a diagnosis earlier means patients can begin treatment earlier.
“This translates into better care,” says Dr. Bailly. “A delay in a diagnosis of cancer could equate to a poorer outcome.”
Dr. Bailly knew that having MRI fusion technology at the QEII would enhance its position as a regional centre of excellence in the detection and treatment of prostate cancer. Currently, most academic health sciences centres in Canada and the United States offer the technology, which has been around for about seven years.
Dr. Bailly initially went to the department of diagnostic radiology, and together, he and the department started to build a collaborative team to find a way to bring the advanced technology to the QEII.
“This is a perfect example of collaborative efforts that identified a need,” says Dr. Bailly.
The QEII Foundation got on board and with its support donors raised approximately $450,000 of the $600,000 cost of the new equipment and software needed to go with it.
“QEII Foundation donors continue to step up and help health care in the region reach new heights,” says Susan Mullin, the QEII Foundation’s president and CEO. “The real impact of this milestone is the patients who are accessing the best treatment with the hopes of the best outcomes possible.
“We are grateful to work with donors who share our vision to transform health care, and today’s new treatment for prostate cancer is just one example of philanthropy at its best.”