Cutting-edge technology is giving QEII Health Sciences Centre clinicians a close up look at the inner workings of the human ear.
“We are the only place in the world that has managed to measure ear vibrations in humans. We are definitely the furthest ahead,” says Dr. Manohar Bance, QEII ear surgeon. When it comes to middle ear dysfunctions, surgeries to cut open the tympanic membrane, or eardrum, are frequently conducted on patients in attempt to identify problems and restore vibrating connections.
Anything that can block the passage of vibrations will lead to hearing loss.
Fluid is one thing, which is common in children, bones get stuck, and cancers can also prevent vibrations.
Unfortunately, current procedures can result in complications. Sometimes, doctors are unable to identify why the ear is not functioning properly leaving them wondering what went wrong.
These unsuccessful surgeries lead both patients and doctors down a long road of surgical exploration in order to identify the problem and develop treatment options.
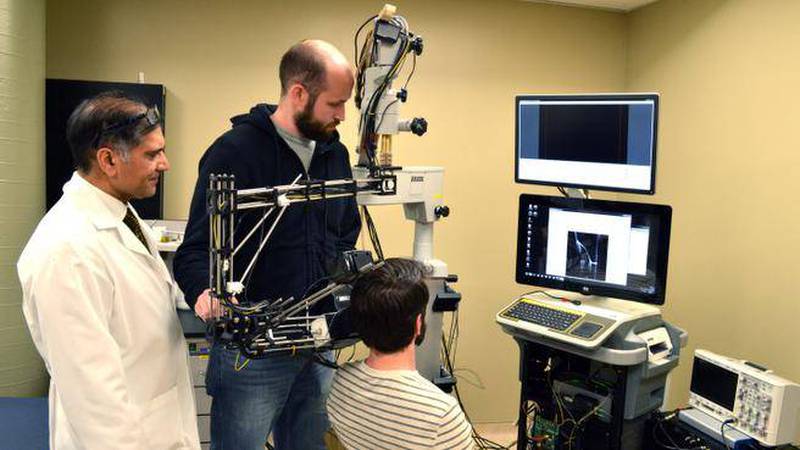
Optical coherence tomography (OCT) was originally developed for retinal imaging, where it continues to be widely used. However, a team of doctors and biomedical engineers at the QEII have developed a microscope to see into the middle ear by scanning a laser beam down the ear canal and through the eardrum.
“The eye is made to transmit light, which is why OCT works so well. The ear is not,” adds Dr. Bance. “But it does use the same physics principles. The eardrum is translucent and this technology sees through that very well.”
This new OCT technology will enable doctors to see 3D images of the tiny bones which make up the middle ear and watch them vibrate. This provides increased visibility of the blockages in the pathway of the vibrations.
The primary function of the new technology is to allow for a quicker, clearer understanding of middle ear problems leading to easier diagnosis and more informed therapeutic decisions.

The OCT device produces a detailed map of the middle ear and then translates it into a 3D image. (QEII Foundation)
“The point is to make the technology portable, maybe even handheld, so it can be taken to wherever people are, from home visits or front line workers. In the developing world in particular there are a lot of middle ear problems,” explains Dr. Bance.
Dr. Rob Adamson, a biomedical engineering professor at Dalhousie University, is heading the research with a team of graduate engineering students.
He says applying OCT technology for the middle ear required a complete redesign.
“You only need a couple millimetres for a retina to be readily visible. The ear, although relatively small, is actually really big for this type of imaging, since you want to generate an image that is about one centimetre cubed,” explains Dr. Adamson.
“We are trying to give clinicians the kind of view they would have in the operating room, but in the clinic without having to do a surgery.
This technology will allow for more informed therapeutic decisions.”
Dr. Bance says two grants from the Atlantic Innovation Foundation made the development of this technology possible. The first grant provided him the opportunity to hire two biomedical engineers in 2006 to create a bone conduction device to hear through skull vibrations.
Subsequently, a second grant was awarded to begin redesigning OCT for middle ear imaging, as well as a separate research project to develop high frequency ultrasound imaging of the ear.
Currently, the technology is in clinical trials within the clinic and has recently been advanced with the addition of a camera that allows for increased external visibility.
Dr. Bance explains the curvature of the ear canal varies from person to person, which created challenges in navigating the curves to be able to see the eardrum. At this stage, he says, they are “validating what the technology can and cannot do,” within the Sensory Encoding and Neuro-Sensory, or SENSE lab, at the QEII. The SENSE lab integrates engineering and physiology in hearing and balance.
“It is revolutionary technology if it takes off and every clinic that does any ear stuff will want one if we make it work. It is a brand new direction,” Dr. Bance says. “The technology is working, now we just need to prove the clinical utility.”