In November 2016, Andrea Cote went to her family doctor with a troubling mystery.
“I was really fatigued all the time. I found it really hard to concentrate and was always exhausted. I could sleep 17 hours and wake up exhausted,” she says.
Her doctor sent her for bloodwork, which determined her iron was abnormally low. Andrea’s doctor sent her to Dr. Stephen Workman, interim division head of the QEII Health Sciences Centre’s Division of General Internal Medicine. He did more bloodwork and asked her more questions, rather like a detective trying to solve a crime. They realized Andrea, 46, had endured varying intensities of the exhaustion since her 20s.
He had her take iron pills, but they didn’t solve her mystery. “That increased to six iron infusion treatments from January to March 2017. I really noticed a difference,” Andrea says. “I actually felt present in my life, where before, I was just going through the motions.”
Speaking after a recent follow-up visit to Dr. Workman, Andrea says her life has transformed.
“I can’t believe I fought through my whole life like I was living in a bowl of oatmeal. Now, I don’t have to hit the snooze button for two-and-a-half hours.”
Andrea’s blood work tested positive for celiac disease, a contributor to anemia. Since her diagnosis, she has changed to a gluten-free diet and is experiencing positive results. “I can’t believe this is how people feel all the time! It’s amazing,” she says.
Her story is a familiar one in the General Internal Medicine Clinic. Its specialists diagnose and manage diseases of any organ system and are specially trained to manage patients with advanced illness or conditions involving more than one system or organ, such as hypertension, heart failure, vascular and allergy/immunology.
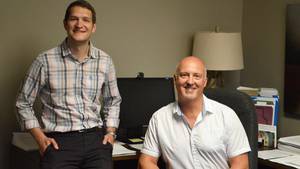
Dr. Workman and Dr. Ashley Miller, a general internist and director of outpatient care for internal medicine, says they connect patients coming from a family doctor to the wider expertise at the QEII. “In some cases, that’s because they have many complex medical problems and they’d like a general internist who can look at all of those problems in totality,” Dr. Miller says.
Many of their patients have “symptom complexes that are undifferentiated,” which means the person has lots of symptoms, but no one knows why. “And rather than having them see three or four people to go at each problem in isolation,” they go to the clinic for a big-picture assessment.
Dr. Workman says modern medicine can do a lot of things, and often the default setting is to do them. “But choosing the ones that are most important and will return the biggest value to the patient takes experience with multiple diseases and a lot of time spent with patients and their families.”
Doctors at the General Internal Medicine Clinic help patients decide which treatments to pursue. Dr. Workman says an older patient with a narrowing of the blood vessel connecting the neck and brain might decide to live with it if the treatment involves short-term risks for long-term gain.
Dr. Miller says solving mysteries like Andrea Cote’s constant fatigue is what drew her to the field after a career as a family doctor. “General medicine uniquely allows you to consolidate all of the areas of medicine that we’re trained in,” she says. “There’s a very strong focus on lifestyle modification in our clinic. Looking at things from a preventative perspective — exercise, good nutrition, mindfulness, stress reduction — these tend to have very strong preventative qualities and can also be very therapeutic.”