Twenty-eight years ago, Nova Scotia’s first heart transplant was performed at what is now the QEII Health Sciences Centre. Today, used to treat severe, end-stage heart failure, QEII cardiac surgeons usually perform five to 10 heart transplants each year. But this spring, something special happened – three people received new hearts within a three-week period.
Steve Gordon, of Saint John, N.B. was one of them. Steve had faced health challenges for years. “I’d had six heart surgeries including having valves replaced and nothing was working. They put me on the transplant list and gave me the pump,” he says.
The pump Steve is referring to is also known as a Left Ventricular Assist Device or LVAD. It is just one technological advance that has significantly changed the lives of heart patients. In fact, QEII cardiac surgeon Dr. Roger Baskett says some people choose to live with one of these rather than opting for a transplant, a complex surgery.
“Heart transplant surgery involves the removal of a failing heart, including any implanted devices such as LVADs, defibrillators or pacemakers, and replacing it with a donor heart,” says Dr. Baskett.
In Steve’s case, the LVAD wasn’t enough as it was not ‘cooperating’ with his defibrillator.
“When I had the transplant, it was like someone turned a switch on,” he says. “I’ve had some of the best months I’ve had in years.”
Pamela Gaines of Dartmouth, N.S., had cancer a little over five years ago and in most cases, this would have disqualified her from transplantation. However, when she developed heart failure two years ago, she had a defibrillator implanted. Because Pamela’s heart failure occurred on the right side of her heart, she was not a candidate for a LVAD. As her condition continued to deteriorate, Pamela’s healthcare team at the QEII managed her condition and placed her on the transplant list.
“By the fall of 2015, my body couldn’t manage all the excess fluids,” she says. “And I was ‘paddling down denial’ despite the reality of life getting more challenging. But this spring, I got the call.”
She was lucky — a heart that was small enough to fit her frame and of the right blood type was available. Following the transplant surgery, Pamela awoke to the sound of a healthy heart beating in her chest.
“They said they had never seen a heart synchronize so quickly before,” she says.
For Luc Bernard from Dieppe, N.B., his lucky day came about two weeks later. He received his LVAD in 2015 and, similar to Steve’s experience, it wasn’t working well for him.
“Over the following months, I had repeated blood infections,” he said. “My overall health was declining at a speed that was alarming, to say the least. During a routine visit at the QEII, the transplant coordinator, Kate Storm, pulled me and my wife into her office to inform us they might have a heart for me. After what seemed like days – really five hours – I was told that I was getting a heart.”
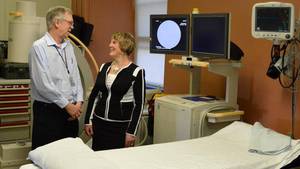
According to Dr. Baskett, there is a lot more to heart transplant surgery than the surgery itself. Patients see various specialists to ensure they are ready for the surgery, both physically and emotionally.
Following transplant surgery, patients remain in hospital for several weeks — depending on their individual recovery — healing and strengthening their new hearts. It was during this time that an already incredible experience became even more special for Steve, Pamela and Luc.
During their daily prescribed walks within the health centre, this transplant trio formed a special bond. These new friends inspired each other every day, working toward their recovery together.
While each had their own unique experience with its own challenges, this heart trio feels like they were part of something special at the QEII.
As their progress continues to be monitored, Steve, Pamela and Luc echo the same sentiment – they are grateful for the QEII’s advanced heart health teams for saving their lives.