Healthcare professionals are always striving to improve three main areas: quality of care, efficiency of care and patient experience. At the QEII Health Sciences Centre, they have found a way to drastically improve all three — at once.
When it comes to treating skin cancer, in most cases, a high-level dosage of radiation is required to be delivered to a patient’s skin surface. A layer of material, called a bolus, is placed on the surface of the patient to assist in the dosage, but the process has become outdated.
“We’ve had to do this for as long as we’ve been doing radiation therapy for cancer treatment, but the status quo has been something very simple that never worked particularly well,” says Dr. James Robar, chief of medical physics. “It’s a simple piece of rubber called SuperFlab, which has been used for decades.”
With SuperFlab as a bolus, it didn't fit particularly well and led to lower radiation accuracy. It also required the patient to sit for long periods of time while one or more radiation therapists adjusted the bolus as best as they could, which could be invasive and uncomfortable for the patient. All of this was happening in the CT suite, tying up a valuable resource and extending patient wait times.
Dr. Robar spearheaded a team to improve this, with the key solution involving 3D printers.
“What we realized is that because we require a CT scan of the patient anyway — to plan their radiotherapy — we can use that CT scan and generate a 3D-printed object that will fit them very well,” says Dr. Robar. “And it can be done without the patient even being there.”
Kathryn Moran, a radiation therapist who works with Dr. Robar, can attest firsthand how time-consuming the old method was.
“We would lay the SuperFlab on the patient's surface — knowing that every person has different contours, dips and curves — and put pressure on it with tape, linen, and stretchy materials to try and conform it as much to the patient as we can, as any air gaps between the rubber and the patient changes the dosage and how the treatment works,” says Kathryn. “That’s a problem, because we set a patient up with high-precision, are treating them with high precision, and then we bring out tape and linen. Patients notice this.”
Now, some patients are able to receive radiation treatments with a bolus made of a customized, more flexible material, printed specifically to match the unique shape of the body part being treated. And, perhaps even more importantly, it’s not a time-consuming process for either the patient or the healthcare provider.
“Right now it’s an overnight affair to print a bolus, but completely automated,” says Dr. Robar. “We prepare the data and use our own in-house algorithms to design the bolus. Then we press the print button and it is ready in the morning when we come in — it’s quite amazing.”
The process started when looking for a way to improve the dosage of radiation given from electron beam therapy, preferential for treating skin cancer.
“The dose that’s deposited around the volume of the tumour, when using electron beams, didn’t always match the shape of the tumour very well, as tumours aren’t round or rectangular,” says Dr. Robar. “We needed a way to control the intensity of the beam at different parts, ultimately creating a radiation dose distribution in 3D that conforms very well to the tumour, and spares other healthy tissue.”
The result is a novel technology — Modulated Electron Radiation Therapy (MERT) — which implements algorithms and methods developed by Dalhousie University graduate student, Shiqin Su. The technology is also patented, and they are now in the process of licensing.
While this technology is greatly improving patient care, the amount of time saved is transformational.
“Before, it could take up to three hours to build a traditional bolus depending on the complexity — that is not modulated to affect the distribution of the radiation — by using wax, rubber and other items on a patient,” says Kathryn. “Instead, this can be pre-printed, available for the patient when they come in, it fits perfectly, and we can scan them and do the entire process. We saved hours on that one patient's trip alone.”
While currently used on a small number of specialty cases, the use of 3D-printed bolus is only going to increase. As technology improves, the applications are endless. But the one thing that will never change is the healthcare providers’ drive to learn more.
“The concept for the project started with the same thing that keeps us going today,” says Kathryn. “It’s the desire to give better care for our patients.”
What does the 3D printer actually print?
The QEII's 3D printers are creating boluses that are leaps and bounds ahead of the traditional material used, the inefficient SuperFlab. But what exactly are the materials now being used, which are more flexible and form-fitting to meet the patients’ needs?
“We have three different materials we print boluses with. We start with PLA — Polylactic Acid — which is a derivative of starches, such as corn, tapioca or sugar,” says Dr. Robar. “It’s similar to what many personal water bottles are now made of, and is non-toxic and bio-compatible. It’s already being used for surgical screws.”
Dr. Robar realized, however, that they also need materials with even more flexibility.
“If the patient moves slightly, we want the bolus to move with them, so we have a material called NinjaFlex,” says Dr. Robar. “In the middle of the two we also have SemiFlex, which we will likely use the most, as it has a very good balance of flexibility and firmness.
“We also have special printers that can print with multiple materials, so the same 3D printer can print with different materials at the same time.”
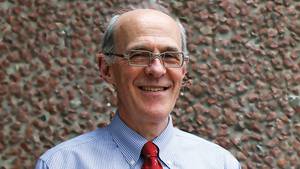
Photo caption: Kathryn Moran, radiation therapist and Dr. James Robar, chief of medical physics, examine a bolus used in radiation treatment for cancer. The bolus was created with one of the QEII’s 3D printers. (QEII Foundation)